ARTICLE OVERVIEW: Detoxing from Vicodin is uncomfortable, but rarely life-threatening. This article will guide you through the medical process and explain what you can expect.
ESTIMATED READING TIME: 7 minutes.
TABLE OF CONTENTS:
- Your Brain on Vicodin
- Becoming Physically Dependent
- What Detox Is Really Like
- Detox Complications
- Duration
- Timeline
- Dangers
- Can You Detox Yourself?
- Where To Detox?
- Medications
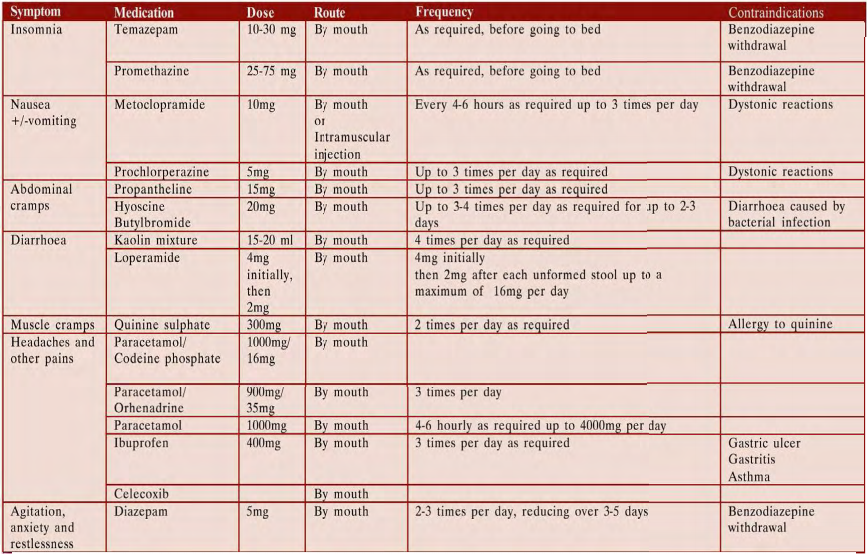
- Treating Common Symptoms
- Your Questions
Your Brain on Vicodin
The precise mechanism of action of hydrocodone and other opiates is not known, although it is believed to relate to the existence of opiate receptors in the central nervous system. Hydrocodone works by flooding opioid receptors in the brain, which is why you experience blocked pain, and increased serotonin that gives you a relaxed and pleasant feeling throughout the body. It works by changing the way the brain and nervous system respond to pain. The analgesic action of acetaminophen involves peripheral influences, but the specific mechanism is yet undetermined.
It is important to see your doctor if Vicodin is no longer working for you. Call us to learn more about getting off Vicodin for good.
Becoming Physically Dependent
Withdrawal occurs because the brain is trying to compensate for no longer having hydrocodone in the system. During withdrawal, the body tries to reconfigure chemistry in the pathways of the brain to stabilize the central nervous system and get the body back to normalcy. It can happen any time you’re physically dependent on Vicodin and you miss a dose of Vicodin or choose to quit taking it.
What Happens To Your Body And What It’s Really Like?
When the withdrawal process starts, you will begin to feel several symptoms that mimic the flu. This will make you very sick for a time. Along with the “flu”, there are other symptoms, which may accompany withdrawal. In some cases, more serious psychological symptoms, such as hallucinations or suicidal thoughts, may occur.
Symptoms of Vicodin withdrawal usually aren’t life-threatening. However, they can be unpleasant. Initial symptoms include:
- Anxiety and agitation.
- Cramps.
- Diarrhea.
- Insomnia.
- Muscle aches.
- Nausea.
- Runny nose.
- Sweating.
- Vomiting.
- Yawning
The time it takes for withdrawal symptoms to start differs person to person. Both long-term and short-term use of Vicodin can cause symptoms.
Detox Complications
- Aspiration.
- Cardiac arrest.
- Drug relapse.
- Excessive vomiting and diarrhea, causing dehydration.
- Psychosis.
- Seizures.
When any of these complications arise, seek medical help at soon as possible.
It is recommended that you try to avoid withdrawal side effects. You don’t have to needlessly go through the pain and uncomfortably of withdrawal if you don’t have to. Tapering your doses of Vicodin allows your body time to heal and slowly regulate itself. With each decreasing dose, your body adjusts without going into a panic.
Duration
Timeline
24 – 72 Hours
You begin the rocky road of detoxing from Vicodin. It will be some of the hardest hours you may experience. Withdrawal symptoms you will go through may include muscle spasms, chills, diarrhea, anxiety, and fear. Symptoms reach their peak during this time and stabilizing your body can feel like a very, very bad flu.
Week 1 Vicodin Withdrawal
Onset symptoms will carry over into days 3-7 as they continue to peak in intensity. Symptoms to expect are severe insomnia and mood swing, which will continue to affect you. Also extreme fatigue as your body exerting a lot of energy to repairs itself.
Week 2 Vicodin Withdrawal
You will begin to see a difference in your body and perhaps your mood. Your body is slowly returning to normal and withdrawal symptoms begin to even out and slowly decrease over time. Appetite should be returning to normal as well. However, you may still experience muscle aches and pains.
Week 3-4 Vicodin Withdrawal
During this time, you may notice continued problems with sleep or mood. Sometimes, sleeping can be difficult or fitful. Some people experience anxiety or depression. And if you are addicted to Vicodin, staying away from hydrocodone can challenging do to drug cravings and drug seeking behaviors.
Dangers
For long-term users, relapse after withdrawal can be deadly. Many who want to take the drug “just one last time,” will consume it at the normal rate they tolerated prior to withdrawal. Because the drugs are out of their system, this amount can prove too much for the brain to handle, so that, many people overdose.
Symptoms of overdose may include the following:
- Cold, clammy, or blue skin.
- Excessive sleepiness.
- Loss of consciousness.
- Narrowed or widened pupils.
- Seizures.
- Slow, shallow, or stopped breathing.
- Slowed or stopped heartbeat.
Moreover, relapse can result in the worst side effect… Death.
Naloxone is used to reverse the life-threatening effects of an overdose. It works by blocking the effects of opiates to relieve dangerous symptoms caused by high levels of opiates in the blood. You will probably be unable to treat yourself if you experience an opiate overdose. You should make sure that your family members, caregivers, or the people who spend time with you know how to tell if you are experiencing an overdose, how to use naloxone, and what to do until emergency medical help arrives.
Can You Detox Yourself?
If you have just started taking Vicodin, for example, and expect a minimal withdrawal period, you may be eligible. However, for others who have taken Vicodin for more than a few weeks, medical supervision is strongly recommended to help address side effects. Additionally, drug cravings make it difficult to continue when you’re detoxing on your own.
Where To Detox?
A variety of treatment options are available, including specialized detox clinics, inpatient rehabs, and outpatient clinics. As with any medical decision, weighing the advantages and disadvantages of each setting with a qualified addiction treatment professional can help assure that an effective treatment type is selected.
Specialized Detox Clinics
In fact, a physician should be available 24 hours per day by telephone and should provide onsite monitoring of care and further evaluation on a daily basis. The types of residential detoxification programs provide 24-hour supervision, observation, and support. Peer and social support may also be included, with 12 Step Meetings or participation in therapy.
Inpatient Rehabs
- Regular eating times.
- Regular sleeping times.
- Structured routine and daily schedules.
- Talk therapy.
You are committed full-time when enrolled in this type of treatment program, which can engage you in daily activities for 6-8 hours a day. The duration of treatment is most effective when it is a full 30-90 days long. Heavier Vicodin usage results in a longer rehab stay.
Outpatient Clinics
Medications
The following medications are using during Vicodin detox:
Buprenorphine works similarly to methadone, but it does not require the same sort of oversight in clinics, and it has less potential for abuse. It can be prescribed to persons working in both inpatient and outpatient rehabilitation programs, with a physician’s oversight to taper doses until the person has been successfully weaned off all opioids. Buprenorphine binds to the opioid receptors in the brain for longer than other opioid drugs, which helps to ease withdrawal symptoms and satisfy cravings without creating a “high.”
Although clonidine was developed to treat high blood pressure, it is often prescribed for people detoxing from an opioid addiction to help ease the fight-or-flight response in the brain. This medication may ease certain symptoms of withdrawal, such as sweating, restlessness, and anxiety.
Methadone relieves withdrawal symptoms and helps with detox. It is also used as a long-term maintenance medicine for opioid dependence. After a period of maintenance, the dose may be decreased slowly over a long time. This helps reduce the intensity of withdrawal symptoms. Some people stay on methadone for years.
Naltrexone, an opioid antagonist, stops opiates like Vicodin from binding to the brain’s receptors. This medication is typically not used until after a person has successfully detoxed from their addiction. It is used instead as a method to help maintain sobriety by preventing opioid drugs taken during a relapse from having an effect.
Suboxone is another medication for Vicodin addiction treatment. This medication is a combination of buprenorphine and naloxone, which is designed to lower the potential for abuse. When ingested as prescribed, Suboxone’s buprenorphine component works on the brain to ease withdrawal symptoms and cravings; however, when crushed or abused in ways not as prescribed in order to get high, naloxone binds to the opioid receptors in the brain instead, stopping the uptake of all other opioids and sending the person into withdrawal.








Related Posts