ARTICLE SUMMARY: These guidelines will help you bring hope and healing to clients who may be in the midst of a battle with opioid addiction and dependency, stemming from chronic pain.
ESTIMATED READING TIME: 7 Minutes.
TABLE OF CONTENTS
- The Need to Talk
- Meet Clients Where They Are.
- Understand Trauma and Talk About It.
- Teach About Opioids and Chronic Pain.
- Educate on Alternative Pain Management.
- A Call to Action
The Need to Talk
Chronic pain, which is one of the leading drivers of opioid overprescribing and subsequent addiction, affects 133 million Americans and 65% of them seek care for persistent pain at some point in their lives, reports the American Cancer Society. And the National Institutes of Health reports that an estimated $100 billion is spent annually to manage pain, including healthcare expenses, lost income, and lost productivity at work and home.
Since this is an issue that impacts many families, friends colleagues, and loved ones in every stretch of the country, I’ve developed some tips for opening honest dialogue about this issue for healthcare professionals, clinicians and therapists to talk with their clients.
Guidelines for Talking to Clients
As a clinician and interventionist, I know first-hand how it can be difficult to broach this topic in an informed and compassionate manner. However, with these guidelines you’ll be able to bring hope and healing to clients who may be in the midst of a battle with opioid addiction and dependency, stemming from chronic pain.
1. Meet Your Client Where They Are.
This approach also leaves judgment at the door. Addiction – in all its forms – is a disease, not a moral failing, and should be discussed in terms of the best way to bring healing to the person experiencing the disease. When we do this, we see the person for who they are and that can open the door to recovery.
2. Understand Your Client’s Trauma and Talk About It.
Trauma can be both objective and subjective:
- Objective trauma is the event that took place
- Subjective trauma is how the person perceives what took place and the emotional aftershocks
When we understand and discuss the trauma that took place, we then see how the door was opened to an opioid misuse problem. For example, a client may be a collegiate baseball player who tore his rotator cuff during a game. He undergoes two surgeries to fix the rotator cuff and is prescribed pain killers to aid in the healing process. But the player does not want to miss any more games, so he misuses the amount of painkillers he should take in order to “play through the pain” and stay in the game. As such, he develops an addiction and continues to take pills long after the rotator cuff healed. That you discuss the trauma in relation to the client’s pressure to succeed as a baseball player illuminates a detailed treatment plan for recovery.
3. Teach Your Clients About Opioids and Chronic Pain.
- The National Survey on Drug Use & Health found that 92 million US adults, or about 38 percent of the population, took a legitimately prescribed opioid like OxyContin or Percocet in 2015. Prescription opioids are easy to come by and are impacting people from all walks of life.
- 11.5 million people, or nearly 5 percent of the population, misused prescription opioids they obtained through illicit means.
- In 2015 more than one third of all adults were prescribed opioids.
- Over 259 million prescriptions were written in 2012, which is enough to give nearly every person in the US regardless of their age their own prescription bottle
- A study authored by Bradley Martin, a professor of pharmaceutical evaluation and policy at the University of Arkansas for Medical Science, found that with a one-day supply of prescription painkillers, there’s about a six percent chance “of being on opioids for a year or longer.” A five-day supply jumps to 10 percent. And a ten-day supply bumps the user to a 20 percent chance they’ll still be using a year later.
- Pain has been considered the fifth vital sign. That being said, 90 percent of all pain is emotion.
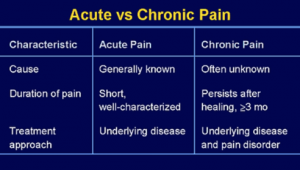
- The differences between acute & chronic pain. See chart below:
4. Educate Your Clients on Alternative Pain Management Solutions.
- CBT
- Breathing exercises
- Qi chong
- Physical therapy
- Acupuncture
- Mindfulness
A study published in the journal Addiction in 2016 by a team from the Veterans Administration Ann Arbor Healthcare System’s Center for Clinical Management Research found a non-drug approach that combines psychological therapies with a social element. In the study, 55 veterans took part in therapy rooted in the psychological theories of pain and felt the effects last up to a year.
The theory behind this approach is a self-management of pain. According to Medline Plus, the person experiencing the chronic pain needs help learning to think, feel, and do better, despite the persistence of pain. Self-management programs engage the individual in problem-solving, pacing, decision-making, and taking action to manage their pain. And they do it in a supportive environment where the social element plays a huge role because research shows that there is a link between pain and depression. Pain is responsive to mood and mood is responsive to social support, thus working through pain in a social environment posts strong results in healing.
With research showing that the support of others aids in recovery, centers willing to address the issues of pain management and recovery, and the medical community rethinking how opioids are prescribed, there are new ways developing to more effectively deal with chronic pain and the mental health and lifestyle issues that arise from these conditions.
Another alternative pain management solution that is gaining traction is meditation. Scott Weiss, clinical director at Bodhizone Physical Therapy and Wellness in New York City, who works with professional athletes, regularly prescribes meditation. “People often find meditation hard to swallow,” Weiss tells Outside Magazine, “but with the right instructor, they can start finding relief in just one session.” In fact, Weiss claims that half of the injured athletes he sees use meditation, and of those, 80% report reduced pain.
A Call to Action
If you have a client that is experiencing difficulty with depression, anxiety ,chronic pain and/or opioid misuse, please give me a call. There is hope and solutions!








Related Posts