As we grew old, we were taught that substances of abuse were lurking through the intercity, waiting to pounce upon us from downtown intersections or head shops draped in burglar bars. As we grew older, we realized that this, alone, was far too romantic. In reality, the one-off hydrocodone prescriptions that were never strong enough for our wisdom tooth pains were incubating in our medicine cabinets like Christmas candy. The blueprint outlined on our health class chalkboards described a character flaw – an unconscious loyalty to the heroin manifesto. America’s addiction to prescription opioids is an unwritten, unadvertised project. One day, it just happened.
So, what can Prescription Drug Monitoring Programs (PDMPs) do about this issue? PDMPs empower prescribers and dispensers with prompt access to patients’ controlled substance prescription histories, providing improved avenues to early interventions for at-risk, abuse-prone populations. Learn more here, and feel free to post any additional questions at the end of the page.
What are Prescription Drug Monitoring Programs?
The National Alliance for Model State Drug Laws (NAMSDL) describes a PDMP as:
“a statewide electronic database that collects designed data on substances dispensed in the state.”
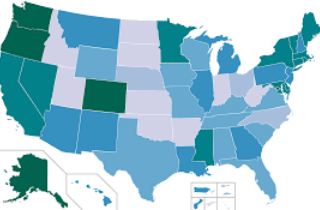
Hence, PDMPs are housed within statewide regulatory, administrative, or law enforcement agencies. Most participating states place PDMPs in a health department, single state authority on drugs and alcohol, professional licensing department, or board of pharmacy. Currently, 49 states and the District of Columbia have established PDMP-like programs (while it has been tirelessly debated in the Senate, Missouri currently does not host a PDMP).
States hosting PDMPs utilize various mechanisms to enact and operate their programs including:
- public and private grants
- state appropriations
- state controlled substance registrations
- direct support organizations
- licensing fees for prescribers, dispensers or manufacturers
Licensing fees are one of the most common funding mechanisms as 17 states receive at least partial funding for PDMPs through licensing.
PDMPs are designed for effective tracking and reporting
Additionally, many states have introduced advisory committees, councils, tasks forces, or work groups that advise the housing entity on matters related to program effectiveness, data entry and accessibility, and data transfer. Other programs exist that report directly to the state legislature regarding the effectiveness of statewide PDMPs in minimizing prescription drug abuse. A particularly sensitive issue to the operation of PDMPs is consumer compliance and confidentiality.
Currently, 11 states require prescribers and/or dispensers to notify consumers that PDMP information is accessible to and reportable by other entities. However, it is punishable by law in 40 states to wrongly disclose, use or obtain prescription monitoring program data.
How can PDMPs prevent prescription opioid abuse?
The 2014 National Survey on Drug Use and Health revealed that 50.5% of people who misused controlled prescription opioids received them from a friend or relative for free. However, only 22.1% of individuals received these same drugs from a prescribing physician. While prescription opioids have been historically effective in the management of moderate to severe chronic pain, the apparent abuse potential of this drug class warrants an increase in rigor with respect to monitoring and cataloging patients’ prescription drug histories.
In 2013, 207 million opioid prescriptions were dispensed by retail pharmacies in the United States, and almost 100% of the total hydrocodone consumers in the world reside here. Thus, America’s addiction to opioids is well established, and a recent national trend of a switch from prescription opioids to heroin may be fueled by deficits in drug diversion control and consequential prescription opioid accessibility.
These harrowing statistics beg for transparency in patients’ controlled substance prescription histories, an essential component to the optimization of opioid prescribing and clinical practice as well as the protection of patients susceptible to prescription opioid abuse. Uniform access to progressive prescription histories emboldens prescribers to identify high-risk, abuse-prone individuals that would benefit from early interventions.
What are the signs of an at-risk patient?
For prescribers and physicians to facilitate interventions for patients with disreputable prescription drug histories, establishing criteria for the identification of at-risk patients is critical. Individual differences in addiction susceptibility are detectable, and one of more of the following risk factors for prescription drug abuse may apply to at-risk patients:
- Past or present addictions to substances including alcohol or tobacco.
- Family history of substance use disorder or related addictions.
- Presence of other neuropsychiatric disorders or mental health ailments.
- Ease of access to substance of abuse such as the presence of prescription drugs in the home or workplace.
What are some early interventions known to help potential addicts?
While substance use disorders can rippled the health of individuals, their families, and their communities, early intervention strategies may aid in the prevention of behavioral health disorders. One model of early intervention in substance use disorder is the Mental Health Intervention Spectrum, a continuum of care introduced in a 1994 Institute of Medicine report that includes the following components:
1. Promotion: These strategies foster environments and conditions that promote behavioral health and the ability of individuals to withstand challenges and overcome hardships.
2. Prevention: These interventions are designed to prevent or reduce the risk of developing a behavioral health problem such as substance use disorder. Prevention strategies focus on education surrounding substance use disorder, and they aim to empower at-risk individuals with the attitudes and skills to prevent or change harmful behaviors.
3. Treatment: These services are optimized for individuals in the addiction cycle, and they aim to treat behavioral health problems such as substance use disorder. Treatment and supportive services are provided in a variety of venues including rehabilitation programs, community health centers, hospitals, and support groups.
4. Recovery: With respect to substance use disorder, these services typically support individuals’ abilities to abstain from future drug and alcohol use and to lead productive, successful lives.
Prescription Drug Monitoring Program questions
Would you like to learn more about PDMPs and what can be done to prevent the growing opioid painkiller abuse in the U.S. We welcome your questions in the comments section below and try to provide a personal and prompt response to all legitimate inquiries.








Related Posts