ARTICLE OVERVIEW: Acute withdrawal symptoms last for 4-10 days after dose cessation. However, symptoms such as anxiety, depression, and sleep disturbances can last for weeks or months following initial withdrawal from Vicodin.
TABLE OF CONTENTS
- Who Withdraws
- Onset
- Timeline
- Common Symptoms
- Overall Duration
- Tapering
- Medical Detox
- Medications that Help
- Home Detox
- Safety
- Your Questions
Who Goes Through Withdrawal?
Withdrawal occurs when you have become physically dependent on Vicodin and then significantly lower doses or stop taking it abruptly. So, withdrawal occurs to anyone who wants to quit Vicodin and is drug-dependent.
Drug dependence occurs relatively quickly with Vicodin. Vicodin dependence can occur after just a few weeks of use. Vicodin is a highly effective narcotic used to relieve pain. The brain’s opioid receptors actively bind to the hydrocodone in Vicodin, which means that dependency, and the withdrawal it yields, often occur after daily dosing over the course of a couple or weeks, or more.
At this point, higher doses of the drug may be needed to relieve pain as effectively as it did before. It is important to see your doctor if Vicodin is no longer working for you. You should not take more or less of the drug without your doctor’s consent. In fact, if you are using Vicodin non-medically, you risk overdose, death, and addiction.
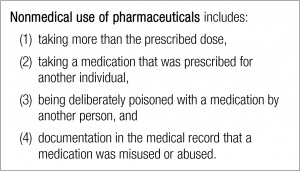
Here is a list of ways Vicodin is used non-medically:
If you have developed a dependency on Vicodin and have decided to stop taking it, you will begin to feel withdrawal symptoms relatively quickly. You will sense these symptoms 6-8 hours after the last dose of Vicodin has worn off. In fact, onset of withdrawal begins when you’re expecting your next dose of Vicodin. You can then expect to experience withdrawal symptoms anywhere from weeks to moths after quitting Vicodin.
Timeline
Everyone is going to go through withdrawal differently. If you have just developed a dependency to Vicodin then detox will be less severe than someone who has been dependent on Vicodin for a long time or has become addicted to it.
When the withdrawal process starts, you will begin to feel several symptoms that mimic the flu. This will make you very sick for a time. Along with the “flu”, there are other symptoms, which may accompany withdrawal. Below is a more detailed timeline of what to anticipate from the withdrawal process.
24 – 72 hours: Vicodin withdrawal peaks during this time. It will also be some of the hardest hours you may experience. Withdrawal symptoms you will go through may include muscle spasms, chills, diarrhea, anxiety, and fear. Symptoms reach their peak during this time and stabilizing your body will be a battle.
Week 1: Onset symptoms will carry over into week one as they continue to peak in intensity. Symptoms to expect are severe insomnia and mood swing, which will continue to affect you. Also extreme fatigue as your body exerting a lot of energy to repairs itself.
Week 2: You will begin to see a difference in your body and perhaps your mood. Your body is slowly returning to normal and withdrawal symptoms begin to even out and slowly decrease over time. Appetite should be returning to normal as well. You may still have aches and pains.
Weeks 3-4: During this time, severe symptoms can return. You may experience some times where withdrawal symptoms wax and wane in severity. If you are addicted to Vicodin these might be challenging do to drug cravings and drug seeking behaviors.
Common Symptoms
Vicodin activates the brain’s opioid receptors, steadily changing brain chemistry and affecting levels of neurotransmitters such as dopamine. These changes mean that your brain cannot feel “normal” without Vicodin, so when you suddenly stop using, you can expect symptoms such as depression and anxiety.
Opioid withdrawal can be dangerous, and symptoms can be severe. In some cases, more serious psychological symptoms, such as hallucinations or suicidal thoughts, may occur. Because the body can also grow dependent on Vicodin, it is common to experience physical symptoms as well.
Early symptoms of withdrawal include:
- Agitation
- Anxiety
- Muscle aches
- Increased tearing
- Insomnia
- Runny nose
- Sweating
- Yawning
Late symptoms of withdrawal include:
- Abdominal cramping
- Diarrhea
- Dilated pupils
- Goose bumps
- Nausea
- Vomiting
Overall Duration
Every person’s body is unique and no two people will go through withdrawal in the same way. Many factors play into recovery. In fact, overall time of withdrawal varies between several weeks and months of stopping Vicodin. Withdrawal can be long but eventually your body will return to normal and you will begin to feel a level of comfort.
It is also important to mention the phenomenon of PAWS, which are post-acute withdrawal symptoms. These are a set of persistent symptoms specific to the type of substance you are taking. In this case, it is specific to opioids. According to SAMHSA’s July 2010 Advisory on Protracted Withdrawal these symptoms mimic the onset of withdrawal at the beginning but they then can last several weeks and months past expected detoxification period.
Protracted withdrawal specific to opioid include:
- Anxiety
- Depression.
- Fatigue.
- Inability to feel pleasure.
- Sleeping problems.
In general, psychological effects of drug dependence take much longer to treat and cure and some many never fully disappear.
Tapering
Depending on the type and dose of drug you have been taking, it may take weeks or even months to gradually and safely reduce your dose and get off Vicodin safely.
If you have taken opioids for less than two weeks, you should be able to simply stop these medications as soon as your prescribed course of pills runs out, if not before. Ask your doctor if you are not sure when you can stop your medications.
If you have taken opioid medications for more than two weeks, you may also need to stop using these medications as soon as possible to prevent serious consequences.
Common signs that it’s time to get off opioids include:
- Behaviors that raise concerns about misuse, abuse or addiction.
- Reduced pain relief from the same dose of medications over time, called tolerance.
- Serious side effect(s).
Do not try to go cold turkey on your own. When it is time for you to stop taking opioids, ask for your doctor’s help to develop a medication withdrawal plan (called a taper) that gradually reduces the amount of medication you take. Opiate withdrawal protocols are fairly straightforward. However, the right length for an opioid taper varies with each person and each medication. Your doctor will prescribe an opioid taper schedule that addresses your medical needs while minimizing risks to your health.
During a taper, your doctor may:
- Ask for your permission to speak with your other health care providers, pharmacist or family members to obtain information that may help with your medication taper.
- Introduce other pain therapies as needed.
- Prescribe other types of medications to help you manage withdrawal signs and symptoms such as sleep, appetite and mood disturbances.
- Regularly monitor your pulse, blood pressure and temperature.
- Request urine or blood samples to check the type and amount of medication or other substances in your system.
Follow your withdrawal plan closely, especially your doctor’s instructions about how and when to take medications during the taper. Although you may be eager to reach your goal, your body needs time to adjust to lower levels of opioids in your body, and then to none at all. A systematic reduction in your dose helps this process go smoothly and helps ease the discomfort you may feel when you stop taking opioids. It also allows you to practice new skills to manage pain and other chronic symptoms.
You may be tempted to take more medication than your taper requires. Do not supplement your taper with additional medications from home, visits to the emergency room, or with alcohol or street drugs. If you feel the need to supplement, contact your health care team.
Talk with your doctor if the taper process becomes difficult. S/He can assist and encourage your success. Your doctor may recommend combining your taper with counseling on medication use. In some cases, you may also wish to join support group or talk with your religious or spiritual advisor.
Medical Detox
Medical detox is the process during which doctors, nurses, and staff supervise detox. They can administer medications, when needed, and treat symptoms as they occur.
Medical detox is important for a few reasons:
- It helps prevent relapse.
- It makes the process more bearable.
- Staff can offer psychological and emotional support.
Medications that Help
Medications are available to help during detox. However, if you have an addiction to Vicodin, medication alone will not help you. According to the National Institute on Drug Abuse, behavioral therapies, counseling, education and treatment medications should all be used to change brain function and reduce cravings. [1]
Anyone going though detox should also be checked for depression and other mental illnesses. Treating these disorders can reduce the risk of relapse. Antidepressant medicines can be given as needed. The most common medications used for Vicodin withdrawal include:
1. Buprenorphine (Subutex) treats withdrawal from opiates, and it can shorten the length of detox. It may also be used for long-term maintenance, like methadone. Buprenorphine may be combined with Naloxone (Bunavail, Suboxone, and Zubsolv), which helps prevent dependence and misuse.
2. Clonidine is used to help reduce anxiety, agitation, muscle aches, sweating, runny nose, and cramping. It does not help reduce cravings.
3. Methadone relieves withdrawal symptoms and helps with detox. It is also used as a long-term maintenance medicine for opioid dependence. After a period of maintenance, the dose may be decreased slowly over a long time. This helps reduce the intensity of withdrawal symptoms. Some people stay on methadone for years.
4. Naltrexone can help prevent relapse. It is available in pill form or as an injection.
People who go through withdrawal repeatedly should be treated with long-term methadone or buprenorphine maintenance.
Most people need long-term treatment after detox. This can include:
- Self-help groups.
- Outpatient counseling.
- Intensive outpatient treatment (day hospitalization).
- Inpatient treatment.
Home Detox
Can I stop taking hydrocodone at home? Possibly, though there are some requirements. You may be able to detox on your own if:
- You are in good general health.
- You have a supportive home environment.
- You have just started taking Vicodin.
- You know which withdrawal symptoms to expect during detox and for how long.
- Your symptoms are not severe.
- You are detoxing with outpatient support from your prescribing doctor.
Still, know that your odds of staying sober without professional assistance are slim. Additionally, if you have taken hydrocodone for more than a few weeks, medical supervision is strongly recommended to manage tapering, because drug cravings make it harder to deal with withdrawal symptoms.
Safety
Anytime you experience withdrawal symptoms, tell a health care professional right away. Follow all instructions you receive about managing withdrawal symptoms.
Unless you are instructed otherwise, you may also find these tips helpful:
- Drink more water or other liquids than usual.
- Eat regular nutritious meals.
- Use deep-breathing and stretching exercises, as instructed.
- Exercise in moderation (for example, walking).
- Do something to relax (for example, practice relaxation techniques, listen to music or read).
- Use distraction (for example, humor, talking to someone with a positive outlook).
- Use positive self-talk. Tell yourself “I can do this” or “This is only temporary.”
Your Questions
If you have any more questions regarding withdrawal from Vicodin, please ask. We do our best to respond to your questions accurately and promptly. You are not alone, contact us. We’ll do our best to help. Privacy guaranteed.










Related Posts