ARTICLE OVERVIEW: Vicodin is an opioid pain reliever and one of the strongest pain medications on the market. Many patients who receive the drug are unaware of the potential dangers behind it. So, what do you do you’ve become drug dependent? How do you withdraw from such a heavy substance and ease symptoms as you go? Learn more here.
Table of Contents:
- What is Vicodin?
- Addictive Potential
- Effects of Withdrawal
- Duration
- Withdrawal Symptoms
- Timeline
- Treatment
- Medications
- Tapering
- Can I Quit Cold Turkey?
- Medical Detox
- Home Detox
- Keep This in Mind
- Safety
- Who Uses Vicodin?
- Your Questions
What is Vicodin?
Vicodin is the brand name for a drug combination of hydrocodone and acetaminophen. It is the second most common opioid drug reported to the DEA. These medications are primarily used to relieve pain, whether mild or severe. To understand Vicodin itself, it’s important to look at these two types of medications in their own respect.
Hydrocodone: By acting upon the central nervous system, this chemical can change the way the brain perceives pain, thereby relieving the most severe of pain. It’s a part of a class of medications known as narcotic analgesics and has strong potential to be habit forming (both physically and mentally).
Acetaminophen: This is a non-addictive medication that’s used for mild cases of pain and to treat fevers. It cannot become habit-forming, even when taken for a long period of time. However, you can overdose on acetaminophen on doses from 4-7 g per day in adults. More on acetaminophen toxicity from Stat Pearls.
Addictive Potential
Vicodin is a Schedule II drug regulated by the Controlled Substance Act. In fact, Vicodin has recently been moved from a Schedule III to a Schedule II drug. As overseen by the Drug Enforcement Agency, Schedule II drugs, substances, or chemicals are defined as:
“drugs with a high potential for abuse, with use potentially leading to severe psychological or physical dependence. These drugs are also considered dangerous”.
Why is Vicodin so addictive?
The reason Vicodin can become so addictive is that its main ingredient – hydrocodone – is an opioid drug. Hydrocodone attaches itself to the opioid receptors in the brain in order to treat pain. These receptors are responsible for transmissions leading into our spinal cord which alert us when pain is there. When cut off, pain ceases to be an issue.
In the case of addiction, opioids like Vicodin chemically alter the pleasure chemicals within us. In fact, hydrocodone causes the release of large amounts of dopamine after consumption. The euphoric effect is one of feeling extremely high for about 4-6 hours. And because people tend to repeat behaviors that bring pleasure, Vicodin is one of the most addictive and effective drugs on the market.
Effects of Withdrawal
Withdrawal occurs when you become physically dependent on Vicodin. Dependence is an expected outcome of regular dosing of Vicodin. It occurs after taking Vicodin daily for a period of at least 2-3 weeks. However, dependence DOES NOT MEAN YOU’RE ADDICTED!
Not everyone who’s prescribed Vicodin will reach a level of addiction. If you’re wondering whether or not you’ve gotten hooked, look into Vicodin addiction symptoms. NIDA explores the difference between drug dependence and addiction here.
So, why do we go through withdrawal?
As already mentioned, the hydrocodone in Vicodin triggers strong effects in the central nervous system. Over time, neurotransmitters and chemicals in the brain must adjust to accommodate the depressant effects of Vicodin. In a way, the brain naturally “speeds up” some functions to balance out the “slowing down” triggered by this opioid.
Remove the drug, and the withdrawal symptoms you’ll experience are actually the body going back to a normal state of balance and function. You experience the “sped up” version of body functions…thus, the gastrointestinal discomfort, difficulty sleeping, and cramps. Still, the body needs time to return to a non-chemical state. This is why withdrawal can be highly uncomfortable and/or painful.
Duration
Classic opioid withdrawal lasts from 4-10 days. The acute phase of withdrawal and the strongest effects usually peak around 72 hours after last dose, with minor effects following anywhere from a week to a month. Cravings and emotional side effects could potentially last longer…with some “protracted withdrawal” symptoms lasting for 6 months, or more.
More on protracted or post-acute withdrawal symptoms from UCLA here.
Withdrawal Symptoms
Vicodin causes similar effects on the brain as other opioid substances, so common withdrawal symptoms are similar to opiates. Since everyone’s body reacts to chemicals differently, you can’t be certain of the exact symptoms you’ll experience. However, the timeline and overall experience have been compared to a very bad flu.
Generally, these are symptoms most common during Vicodin withdrawal:
1. Psychological Changes
- Anxiety
- Confusion
- Irritability
- Mood swings
2. Physical Symptoms
- Diarrhea
- Enlarged pupils
- Goosebumps due to shivering
- Heavy breathing
- Muscle aches/cramps
- Nausea/vomiting
- Salivation
- Sweating
- Tremors
3. Appetite Changes
- A strong desire to intake Vicodin
- A lack of desire to eat, reduced hunger
4. Cold-Like Symptoms
- Chills
- Congestion
- Fever
- Runny nose
- Sweating
5. Sleep Interference
- Exhaustion
- Insomnia
- Restlessness
Timeline
First 12 Hours. According to the Journal of Pain Research, upon taking your last dose of Vicodin, you can expect early withdrawal symptoms to appear within 4 to 6 hours. However, there are some forms of Vicodin which are created for extended release, leaving the user not feeling these early withdrawal symptoms until up to 12 hours.
24 Hours After Last Dosage. Withdrawal symptoms emerge and continue to kick in. It is common to experience insomnia and anxiety. Gastro-intestinal symptoms like stomach cramps, diarrhea, and vomiting are common. You can also expect lots of sweating and a rolling fever.
72 Hours After Last Dosage. The withdrawal levels usually reach their peak. This is where your body and mind will be at its most uncomfortable. When you reach this point, it’s important to remember that it gets easier from here on out. Also know the medical detox can treat symptoms as they occur. So, you needn’t suffer alone.
A Week After Last Dosage: At this point, the body has usually gone back to its normal function or is close to normal. The physical withdrawals have taken their full course. What remains includes mental symptoms of withdrawal, particularly craving. However, they’ll feel less intense than the prior week’s experience. Plus, cravings lessen over time.
A Month After Last Dosage: A lot of people feel much better after a month dree of Vicodin. Though there are some minor mental withdrawal symptoms that still occur, you’ve made it a long way since the first week. Still, there’s still a chance for relapse. In order to prevent this, people take on a variety of treatment options.
Treatment
Vicodin is a powerful drug. It’s extremely difficult to detox and recover from drug dependence on your own. As with other opioids, an inpatient facility is highly recommended during drug withdrawal. As you’ll read later, there are dangers to your health when it comes to withdrawing. Therefore, you’ll need to be under medical supervision throughout much of the process.
Vicodin withdrawal is treated using:
1. Medication
2. Psychological support
3. Emotional support
It can’t be said how long your treatment process will last. Some people manage to come off Vicodin within a few days. For others, it can take the full 10 days to detox. Indeed, there are a lot of factors at play when it comes to success in treatment, such as:
- How strong your support system is.
- Your willpower to get off Vicodin.
- Your environment.
- Your stress levels.
- Your individual rate of metabolism.
But sometimes detox isn’t enough.
Even once the physical withdrawal resolves and the chemicals are entirely out of your system, you’ll have to undergo the mental side of recovery. This is usually hardest for most people, as it requires a lot of self-discipline. Some people just need the extra help. So, detox may lead to a longer stay in a rehab. In fact, many who enter a treatment facility end up finding success, as the additional treatment gives them the opportunity to address underlying issues.
Medications
The World Health Organization has organized clinical guidelines for drug withdrawal. Standard treatment includes 24-7 monitoring, regular patient assessment, and the use of medications. Depending on your specific needs, you’ll most likely be offered either one or more of the following medications during Vicodin detox:
Antidepressants: This type of medication can be used during withdrawal to manage irritability, sleep problems, and mood swings. Short-term prescriptions of 3 months or less can help.
Buprenorphine: This treatment medication is prescribed to help alleviate withdrawal symptoms specific to Vicodin. Additionally, it might be used for long-term support in cases of drug addiction. There are sometimes instances where it can also shorten the length of detox.
Clonidine: When it comes to the minor symptoms of Vicodin withdrawal, clonidine can be a great support. It’s primarily used to reduce levels of anxiety, agitation, muscle aches, sweating, runny nose, and cramping. It has also been known to sometimes act as a sleeping aid and reduce levels of nausea and vomiting.
Methadone: When it comes to an opioid addiction, methadone is a prime medication for handling long-term support. It’s provides relief for withdrawal symptoms and helps with the detoxing process. Usually, people receive methadone and lower the dose over a period of time, during recovery.
Lofexidine: This is an oral tablet recently approved by the FDA, that has been designed to manage the symptoms patients often experience during opioid discontinuation.
Naltrexone: While it doesn’t help with the withdrawal process itself, naltrexone has been known to aid in reducing the chances of relapse. The medication alone doesn’t have the ability to fully rid the potential of relapse, though. And is usually given out when an individual is going through other forms of therapy and counseling.
When it comes to which medications are best to relieve certain withdrawal symptoms, you can take a look at the Clinical Guidelines for Withdrawal Management. Additionally, you can look into the over-the-counter medication necessary for relief. Or, consult your doctor about any prescriptions that may alleviate symptoms.
Tapering
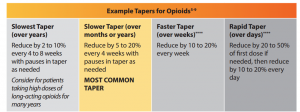
The idea of tapering is that of weaning off Vicodin over a period of time reduces the intensity and severity of withdrawal symptoms. What does it involve? Tapering involves a calendar of dosing and carefully taking less and less Vicodin over the course of several weeks. Gradual dose reduction is seen as a means of avoiding withdrawal symptoms and, eventually, helping you quit for good.
What’s a good rate of dose reduction?
According to the U.S. Veteran’s Association, most tapers used by their organization involve dose reduction of 5% to 20% every 4 weeks. The Utah State Department of Health notes that a decrease by 10% of the original dose per week is usually well tolerated with minimal physiological adverse effects. Some patients can be tapered more rapidly without problems (over 6 to 8 weeks).
Slower, more gradual tapers are often the most tolerable and can be completed over several months to years based on the opioid dose. The longer the duration of previous opioid therapy, the longer the taper may take.
But not everyone will benefit from a taper.
In the case of Vicodin, tapering may be counter-productive, as it can induce cravings. The biggest problem is that many people have trouble controlling themselves when it comes to tapering. Their minds know they shouldn’t take Vicodin, but their bodies crave it. Sometimes, at an overwhelming sensation. Additionally, more rapid tapers may be required in certain instances like drug diversion, illegal activities, or situations where the risks of continuing the drug outweigh the risks of quitting suddenly.
However, you’re still going to want to seek out medical supervision if you’re considering a Vicodin taper. As mentioned, Vicodin withdrawal can be dangerous and should always be medically supervised. If you want the best for your health and safety, a professional can be your guide.
Can I Quit Cold Turkey?
Maybe.
According to Dr. Jennifer Shu of CNN, quitting cold turkey can have some serious risk factors. Though Vicodin’s withdrawal symptoms feature nothing fatal, they have the characteristic of being highly uncomfortable and causing certain mental illnesses, such as depression. Indeed, she considers tapering to be the best option for those about to undergo withdrawal. She notes that it’s very important you undergo the tapering process under the eyes of a medical professional. With a gradual reduction of Vicodin, you’ll allow yourself to avoid certain withdrawal symptoms.
Still, ALWAYS SEEK MEDICAL SUPERVISION when you want to quit Vicodin after a period of drug dependence.
Medical Detox
Coming off Vicodin is best handled in a specialized detoxification center. What are some of the benefits of a medical detox? Within a controlled environment, you’ll be surrounded by a medical staff which offer professional supervision and support. Furthermore, you’ll have access to medical and mental health professionals at all times who can not only assist you in detoxing, but give you the best advice on how to ease withdrawal symptoms. When working with a professional, detoxing is a much safer process with greater chances of success.
Vicodin withdrawals should be monitored when it comes to the following situations:
- Other medical and/or psychiatric problems co-exist.
- There is a polydrug dependence.
- You’re taking a high dosage.
- You’re in need of other medication for the sake of stabilization.
Home Detox
Though an inpatient programming is highly suggested when it comes to the initial physical detox, it’s understandable that some out there don’t have the ability to make such a commitment. Many people who are facing Vicodin dependence still hold the responsibility of day-to-day life and can’t take time off to get to a proper treatment facility.
In this instance, those people will most likely detox from home. Still, even though you can’t commit to staying in a treatment facility, it is a necessity you are under careful medical supervision. Generally speaking, schedule daily check-ins with a supervising physician. Or, plan to have a medical professional check on you regularly.
Keep This in Mind
The best treatment for withdrawal depends on your risk of addiction. To those with little risk of addiction, you might just want to go through with a full withdrawal (depending on how much Vicodin is already in your system). With a low risk, your body most likely hasn’t fully adjusted to the chemicals of Vicodin as it has in people with a high risk. For those individuals, your best options is an initial stabilization and maintenance therapy in specialist residential or an outpatient program.
When it comes to detox management for Vicodin, there are a variety of options to look into. You may even benefit from attending an outpatient drug rehab program. This is for the sake of addressing psychological issues that pertain to your addiction. With this, you can expect to have the responsibility of making daily check-ins with a counselor.
Safety
There are some physical concerns to keep in mind during withdrawal, such as forming an irregular heartbeat and high blood pressure. You’ll also need to drink at least 2 litres of water per day to be sure to avoid dehydration.
Still, the bigger worries come from the psychological changes that occur. Since Vicodin gives off large amounts of dopamine and rewards the pleasure center of your brain, naturally, you’re bound to experience a huge lack of these chemicals. Your brain needs time to rewire itself and flow back into normal functioning. During that time, many people experience large levels of depression and anxiety.
These mental health concerns are known to cause suicidal thoughts. Therefore, it’s important your under medical supervision during the time your brain needs to function properly again.
Who Uses Vicodin?
Most people who start to have problems with Vicodin received a prescription for the pain medication. Many others use Vicodin that the “borrow” from a friend or family member.
But when a doctor gives a patient a drug and that patient goes on to take more than the recommended dosage the risk of addiction increases. Furthermore, with an increase in dosage comes an increase in tolerance. It’s a viscous circle of a need for more and more.
This trend has become more and more common within the last decade. The following statistics show us that the trend is also expected to continue rising.
- In 2010, more than 139 million prescriptions of hydrocodone were filled in the United States alone, making it the most prescribed opiate in the nation.
- Of all hydrocodone medications, the most prescribed are those also containing acetaminophen, such as Vicodin.
- In the 2013 National Survey of Drug Use and Health (NSDUH) found that a little more than 24 million people in the United States, ages 12 and over, used hydrocodone for recreational purposes.
Teens are at great risk of abusing Vicodin, too. According to the 2013 Monitoring the Future survey, around 10% of high schoolers had used Vicodin at one point or another for nonmedical purposes.
So, if you’re experiencing problems…don’t wait.
Reach out for help today.
The earlier you get help, the more likely you are to make a full, drug-free recovery.
Your Questions
So, is it possible for you to quit Vicodin?
Absolutely, yes!
As with many other drugs that are so freely prescribed, it’s not easy. But with the right medical help, there’s no denying your potential to beat this opioid chemical!
Do you still have any questions or concerns about treating Vicodin withdrawal? Please ask your questions in the comment section below. We’ll be sure to get back to you promptly with a personalized response.









Related Posts