ARTICLE OVERVIEW: Hydrocodone dependence can develop after only a few weeks of using the drug daily. Here, we review the ways you can treat hydrocodone withdrawal and what you and your doctor can do to help ease symptoms.
TABLE OF CONTENTS
- What Is Hydrocodone?
- Why Withdrawal Occurs
- Duration
- Symptoms
- Protracted Symptoms
- Medications that Help
- Tapering
- Who Should Not Withdraw
- Why Detox In A Clinic
- Detox At Home
- Safety
- Overdose
- Signs of a Drug Problem
- Who Uses Hydrocodone?
- Dependence vs. Addiction
- Your Questions
What Is Hydrocodone?
Hydrocodone is a part of the opioid family of painkiller drugs which is made in a laboratory, derived from codeine, itself a semisynthetic. The FDA approved its use in 1943, but currently warns against serious harms that the medication can cause. When you take hydrocodone, for example, it can suppress the pain receptors in the brain and the spinal cord, and it may slow the overall body responses.
Opioid medications like hydrocodone have the potential to provide significant pain-relieving benefit for persons when used as directed for their approved indications; however, the CDC warns that opioids also carry serious risks of misuse, abuse, neonatal opioid withdrawal syndrome (NOWS), dependence, addiction, overdose, and death.
Why Withdrawal Occurs
Opioids like hydrocodone work by flooding opioid receptors in the brain, which is why you experience blocked pain. It works by changing the way the brain and nervous system respond to pain. At the same time, you experience increased serotonin surges that give you a relaxed and pleasant feeling throughout the body.
However, over time your body develops a chemical dependency on hydrocodone. This means that the central nervous system adapts to the presence of hydrocodone. It has to, in order to keep working. As hydrocodone becomes part of the normal chemical state, the body responds by “speeding up” certain functions to account for the depressant effects of hydrocodone. This is why when you stop taking hydrocodone, withdrawal symptoms result. They are actually the “sped up” effects that take time to even out again.
The effects of withdrawal occur after the chemical balance of the “hydrocodone state” is interrupted. During this time, opioid transmitters trigger a sort of battle in the central nervous system so that the body can begin to regulate itself without the presence of hydrocodone. In fact, effects of withdrawal from hydrocodone occur as the brain reorganizes its chemical messages. Therefore, hydrocodone withdrawal symptoms occur as your brain and body seek balance after you stop taking the painkiller. In general, withdrawal symptoms are more intense when your hydrocodone prescription dosage has been high.
Duration
Hydrocodone withdrawal symptoms immediately when you miss an expected dose, and generally peak within 12–48 hours after that. In fact, you can expect to feel hydrocodone withdrawal begin shortly after a missed dose. The degree and time that withdrawal takes, however, can fluctuate given your daily dose frequency and amount. Sometime it can take 10–20 days for acute withdrawal to resolve.
However, after you have battled the physical effects hydrocodone withdrawal, you will have to deal with the psychological craving for the drug. Not only can you crave hydrocodone for months or even years after your last use, you may experience:
- Inability to experience pleasure
- Mood disorders
- Problems sleeping
…in the weeks and months after you last use hydrocodone.
Symptoms
Some people take medications and do not become addicted to them but still experience withdrawal if they suddenly stop taking these medicines. In fact, withdrawal is an expected outcome for anyone who take hydrocodone daily for more than a few weeks.
There are a predictable cluster of symptoms that occur for 1-2 weeks when a person stops hydrocodone. The symptoms you may experience withdrawing from hydrocodone may include:
- Abnormal skin sensations.
- Cold flashes with goose bumps.
- Confusion.
- Diarrhea.
- Dilated pupils.
- Excessive yawning or sneezing.
- Extreme drowsiness.
- Fever (temperature over 38,5 ºC 101,3ºF).
- Hypertension (elevated blood pressure).
- Insomnia.
- Involuntary leg movements.
- Lack of appetite.
- Lacrimation, tearing from the eyes.
- Mood changes.
- Muscle and bone pain.
- Nausea.
- Stomach pain.
- Strong drug craving.
- Sweating.
- Tachycardia (accelerated heart rate).
- Tachypnea (accelerated breathing rate).
Protracted Symptoms
Also known as post-acute withdrawal syndrome (PAWS), protracted symptoms of withdrawal refer to any symptoms that persist after a person has ended their physical dependence on a drug. The most common PAWS for hydrocodone include:
- Anxiety.
- Depression.
- Sleep disturbances.
- Fatigue.
- Irritability.
- Deficits in executive control functions.
These symptoms can last for weeks or months following withdrawal from hydrocodone. These can be treated first by having realistic expectations. Understand that it will take time for the brain to achieve balance after long-term drug use. Then, seek a diagnosis for possible mental health disorders which can be affecting you.
Further, look into lifestyle changes. Changes for sleep problems are often beneficial. Engaging in physical and mental exercises which promote positive emotional states can reduce stress and nervousness. Learning new behaviors and habits through cognitive behavioral therapy can help you cope with life without hydrocodone.
Medications that Help
Some treatment centers follow the philosophy that they should not treat a drug addiction with other drugs, but research shows that medication can help in many cases. The FDA has approved a number of drug products that address opioid dependence…but suggests that these medicines are most successful when combined with counseling. Here is a list of the most common SAMHSA suggested medicines used during withdrawal from hydrocodone.
1. Symptom based medicines. Medications like clonidine, Immodium, and among others are used treat specific withdrawal symptoms such as high blood pressure and diarrhea, very common during the acute stage of hydrocodone withdrawal. Other symptomatic medications can be found in this article.
2. Acute withdrawal management. Buprenorphine and meathadone delay withdrawal symptoms and can be used in step-down détox situations.
3. Medication assisted treatment. Buprenorphine and meathadone also relieve psychological cravings that cause chemical imbalances in the body and can be used in the months and years after initial withdrawal. In addiction, nalterxone may be prescribed block the effects of narcotics and is usually taken as a daily pill or monthly injection.
4. New treatments. May 2018, the FDA approved Lucemyra, lofexidine, for the treatment of addiction. This medication is a centrally acting alpha2-adrenergic receptor agonist, presented as an oral tablet, designed to manage the symptoms patients often experience during opioid discontinuation. It is the first non-opioid medication for use in reducing symptoms associated with opioid withdrawal in adults. This could help patients complete their discontinuation of opioids and facilitate successful treatment.
NOTE HERE: Methadone and buprenorphine products are part of the class of extended-release and long-acting (ER/LA) opioids that are approved for the treatment of opioid addiction. This type of treatment is often referred to as “medication-assisted treatment” (MAT) but is underused due to misunderstanding from doctors and the public. When provided at the proper dose, medications used in MAT have no adverse effects on a person’s intelligence, mental capability, physical functioning, or employability.
This SAMHSA mobile phone app will help you find buprenorphine prescribing doctors and learn more about MAT medications and withdrawal options.
Tapering
You do not need to experience needless pain during hydrocodone withdrawal. In fact, the best was to withdraw from hydrocodone is to lower your doses of hydrocodone under medical observation over the course of several weeks. This method allows your body to compensate and slowly regain normalcy. It also minimizes the severity and intensity of withdrawal symptoms.
Tapering down from hydrocodone allows time and space for doctors to address any lingering pain or other health complications that may arise. This CDC guideline for tapering opioids can help. Some general guidelines during tapering include:
- A decrease of 10% of the original dose per week is a reasonable starting point.
- Some people might find even slower tapers 10% dosage decrease per month easier.
- Do not reverse the taper.
- The rate may be slowed or paused while monitoring and managing withdrawal symptoms.
- Once the smallest available dose is reached, the interval between doses can be extended and opioids may be stopped when taken less than once a day.
Tapering hydrocodone doses might not be the best method if you experience an addiction to hydrocodone. In these cases, you may want to stop hydrocodone cold turkey or seek outside non pharmacological help that can address psychological need while also treating physical withdrawal symptoms.
Who Should NOT Go Through Withdrawal
There are some persons who should NOT complete hydrocodone withdrawal. It is recommended that pregnant women who are opioid dependent do not undergo opioid withdrawal as this can cause miscarriage or premature delivery. The recommended treatment approach for pregnant, opioid dependent women is methadone maintenance treatment.
Furthermore, people commencing methadone maintenance treatment do not need to undergo withdrawal before commencing treatment.
Why Detox In A Clinic?
A medically supervised “detox” is a process during which medical professionals supervise the removal of all of the drugs from the system. Supervision is important, because drugs impair the mental abilities you need to stay in treatment.
Detox clinics are also experienced in helping you get through this process and keeping you safe. Not only that, they can provide symptom-based treatments as required. So, you don’t need to suffer through withdrawal.
What can you expect from a medical detox?
Professional staff are available 24 hours a day in a detox clinics. The area is generally quiet and calm. You should be allowed to sleep or rest in bed if you wish, or to do moderate activities such as walking. You should also be provided opportunities to engage in meditation or other calming practices. Counseling or other psychological therapy is not appropriate at this stage.
In a detox, you’ll also be encouraged to drink 2-3 liters of water per day to replace fluids lost through perspiration and diarrhea. Also, vitamin B and vitamin C supplements will be provided. You should be monitored regularly (3-4 times daily) for symptoms and complications. The Short Opioid Withdrawal Scale (SOWS) is a useful tool for monitoring withdrawal. It should be administered 1-2 times daily. Typically, medical detox staff will use the SOWS score to select an appropriate management strategy.
Detox At Home
So, should you consider a home detox?
We ask that you first think about this: repeated drug use changes the brain, including parts of the brain that enable you to exert self-control. These and other changes can be seen clearly in brain imaging studies of people with drug addictions. These brain changes explain why quitting is so difficult, even if you feel ready.
Sometimes people will consider a home detox, or dietary supplement in the hope of getting faster and cheaper help. There are also opiate withdrawal or detox supplements on the market that promise fast results and a path to being drug-free. But, based on the Federal Trade Commission’s past experience, such promises can’t be taken at face value.
If you or someone you know are having drug cravings or a hard time with your emotions, or are tempted to detox at home or use supplements to beat hydrocodone withdrawal, remember that this is a very serious health issue. We suggest that you first speak with a health provider about hydrocodone dependence or addiction. There are effective medical and therapy-based treatments that could help.
You do not need to suffer alone or be afraid during withdrawal.
Safety During Withdrawal
Serious problems can manifest during the withdrawal process such as relapse and overdosing with very dramatic complications such as respiratory deficiency and death. This is because users lower their tolerance for the drug and can provoke an unintentional overdose in an attempt to get high.
Hydrocodone dependence is a serious, difficult and uncomfortable health problems for anyone. If mismanaged, withdrawal can be life-threatening. That´s why it should be addressed with help from a medical professional.
Overdose
Hydrocodone overdose is a reality. So, how can it be treated?
In November 2015 the FDA approved Narcan nasal spray, entered the market to stop or reverse the effects of an opioid overdose. The FDA has also approved a prescription naloxone hydrochloride injection to reverse overdose, which can be used by family members or caregivers to treat a person known or suspected to have had an opioid overdose. This formulation rapidly delivers a single dose of the drug naloxone via a hand-held auto-injector that can be carried in a pocket or stored in a medicine cabinet.
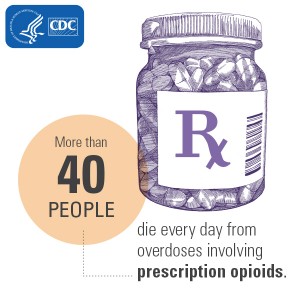
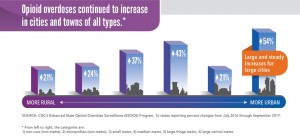
This CDC Vital Signs infographic on opioid overdose illustrates how pervasive the problem is:
Signs of a Drug Problem
Not everyone who takes hydrocodone will develop addiction. however, it happens in about 10% of all users. Addiction is a problematic pattern of hydrocodone use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Taking the drug in larger amounts or over a longer period of time than was intended.
- A persistent desire or unsuccessful efforts to cut down or control hydrocodone use.
- A great deal of time is spent in activities to obtain the hydrocodone, use it, or recover from its effects.
- Craving, or a strong desire or urge to use hydrocodone.
- Recurrent hydrocodone use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued hydrocodone use despite having persistent or recurrent social or interpersonal problems caused by or exacerbated by the effects of hydrocodone.
- Important social, occupational, or recreational activities are given up or reduced because of hydrocodone use.
- Recurrent hydrocodone use in situations in which it is physically hazardous.
- Continued hydrocodone use despite knowledge of having a persistent or recurrent physical or psychological problem that’s likely to have been caused or exacerbated by the substance.
- Tolerance,* as defined by either of the following:
– A markedly diminished effect with continued use of the same amount of hydrocodone.
– A need for markedly increased amounts of hydrocodone to achieve intoxication or desired effect. - Withdrawal,* as manifested by either of the following:
– The characteristic opioid withdrawal syndrome.
– The same—or a closely related—substance is taken to relieve or avoid withdrawal symptoms.
* This criterion is not met for persons taking opioids solely under appropriate medical supervision. Severity: mild = 2–3 symptoms; moderate = 4–5 symptoms; severe = 6 or more symptoms.
It takes a lot of courage to seek help for a drug problem because there is a lot of hard work ahead. However, treatment can work, and people recover from addiction every day. Like other chronic diseases, addiction can be managed successfully. Treatment enables people to counteract addiction’s powerful, disruptive effects on brain and behavior and regain control of their lives.
In 2016, 6.2 billion hydrocodone pills were distributed nationwide.
Who Uses Hydrocodone?
Hydrocodone is the most frequently prescribed painkiller in the United States. There are several hundred brand name and generic hydrocodone products marketed, most of which are combination products. The most frequently prescribed combination is hydrocodone and acetaminophen. According to the DEA,
- In 2013, 136 million hydrocodone-containing products were dispensed.
- In 2014, 65.5 million hydrocodone-containing products were dispensed in the first six months.
- In 2016, 6.2 billion hydrocodone pills were distributed nationwide.
But this access comes at a cost.
About 11.5 million Americans age 12 and older misused prescription pain medicine in 2016, according to the Substance Abuse and Mental Health Services Administration. According to the Drug Abuse Warning Network (DAWN), an estimated 82,480 emergency department (ED) visits were associated with nonmedical use of hydrocodone in 2011. This number of ED visits represents a 107% significant increase from the number of ED visits reported in 2004 (39,846).
Dependence vs. Addiction
Dependence and addiction are two separate medical conditions. Dependence is a condition caused by chronic use of a tolerance-forming drug, in which abrupt or gradual drug withdrawal causes unpleasant physical and psychological symptoms. The basic difference is that people who are dependent can quit…and stay quit. People who are addicted will quit and then return to drug use.
As defined by the American Society of Addiction Medicine (ASAM), addiction is “a primary, chronic disease of brain reward, motivation, memory, and related circuitry.” It is characterized by inability to consistently abstain, impairment in behavioral control, craving, diminished recognition of significant problems with one’s behaviors and interpersonal relationships, and a dysfunctional emotional response. Like other chronic diseases, addiction often involves cycles of relapse and remission.”
Your Questions
We hope to have answered your questions about treating hydrocodone withdrawal…and identifying possible addiction to it. Still have questions about hydrocodone withdrawal treatment? Would you like to know more? Please ask any questions you may have here in the comments section and we will get back to you personally and promptly.




Related Posts